Contents
- Continuous Quality Improvement Tools
- Healthcare Quality Improvement Tools
- Pdsa Description
- Pdsa Cycle Powerpoint Presentations
The Plan-Do-Study-Act (PDSA) cycle is part of the Institute for Healthcare Improvement Model for Improvement, a simple yet powerful tool for accelerating quality improvement. The AHRQ Health Literacy Universal Precautions Toolkit. Create a Health Literacy Improvement Plan: Tool #2. Short Duration—Each PDSA cycle should be as.
On Page 1 of 2:
4.A. Focusing on Microsystems
4.B. Understanding and Implementing the Improvement Cycle
On Page 2 of 2:
4.C. An Overview of Improvement Models
4.D. Tools To Enhance Quality Improvement Initiatives
References
Health care delivery systems that are working to improve patient experience can face daunting challenges, reflecting the need to align changes in behavior and practices across multiple levels and areas of the organization. But the process of planning, testing, and eventually spreading those changes does not have to be overwhelming. Health care organizations can take advantage of established principles and approaches to quality improvement, which are already familiar to the many providers involved in clinical quality improvement (QI).
This section of the Guide suggests a way to use the concept of microsystems to focus the QI process on the locus of responsibility for patient experience, provides an overview of the process of quality improvement, discusses a few well-known models of quality improvement, and presents a few tools and techniques that organizations can use to address various aspects of patient experience.
Three Tips for Facilitating the Quality Improvement ProcessPlace a priority on encouraging communication, engagement, and participation for all of the stakeholders affected by the QI process. Learn what is most important to the people who make up the microsystem and look for ways to help them embrace the changes and begin to take ownership of them.
Start your implementation of improvements with small-scale demonstrations, which are easier to manage than large-scale changes. Small-scale demonstrations or small tests of change also allow you to refine the new processes, demonstrate their impact on practices and outcomes, and build increased support by stakeholders.
Continuous Quality Improvement Tools
Keep in mind and remind others that QI is an iterative process. You will be making frequent corrections along the way as you learn from experience with each step and identify other actions to add to your strategy.
4.A. Focusing on Microsystems
One useful way for health plans and medical groups to approach the process of improvement is to think of the organization as a system, or more specifically, as a collection of interrelated 'microsystems.' The term 'microsystems' refers to the multiple small units of caregivers, administrators, and other staff who produce the 'products' of health care—i.e., who deliver care and services on a daily basis.
The concept of microsystems in health care organizations stems from research findings indicating that the most successful of the large service corporations maintain a strong focus on the small, functional units who carry out the core activities that involve interaction with customers.1 In the context of health care, a microsystem could be:2
- A core team of health professionals.
- Staff who work together on a regular basis to provide care to discrete subpopulations of patients.
- A work area or department with the same clinical and business aims, linked processes, shared information environment and shared performance outcomes.
Examples of microsystems include a team of primary care providers, a group of lab technicians, or the staff of a call center. In the patient-centered medical home model, a microsystem could be the patient's care team accountable for coordination of the patient's services that address prevention, acute care, and chronic care.3
The goal of the microsystem approach is to foster an emphasis on small, replicable, functional service systems that enable staff to provide efficient, excellent clinical and patient-centered care to patients. To develop and refine such systems, health care organizations start by defining the smallest measurable cluster of activities.
Once the microsystems have been identified, a practice or plan can select the best teams and/or microsystem sites to test and implement new ideas for improving work processes and evaluating improvement.5 To provide high-quality care, the microsystem's services need to be effective, timely, and efficient for all patients,4 and preferably designed in partnership with patients and their families.
Measurement and performance feedback must be part of the microsystem's principles to learn and improve.6
If a quality improvement intervention is successful for a microsystem, it can then be scaled to other microsystems or the broader organization. However, for successful scalability, organizations should adopt a framework for spread that will work within their structure and culture.
4.B. Understanding and Implementing the Improvement Cycle
Although QI models vary in approach and methods, a basic underlying principle is that QI is a continuous activity, not a one-time thing. As you implement changes, there will always be issues to address and challenges to manage; things are never perfect. You can learn from your experiences and then use those lessons to shift strategy and try new interventions, as needed, so you continually move incrementally toward your improvement goals.
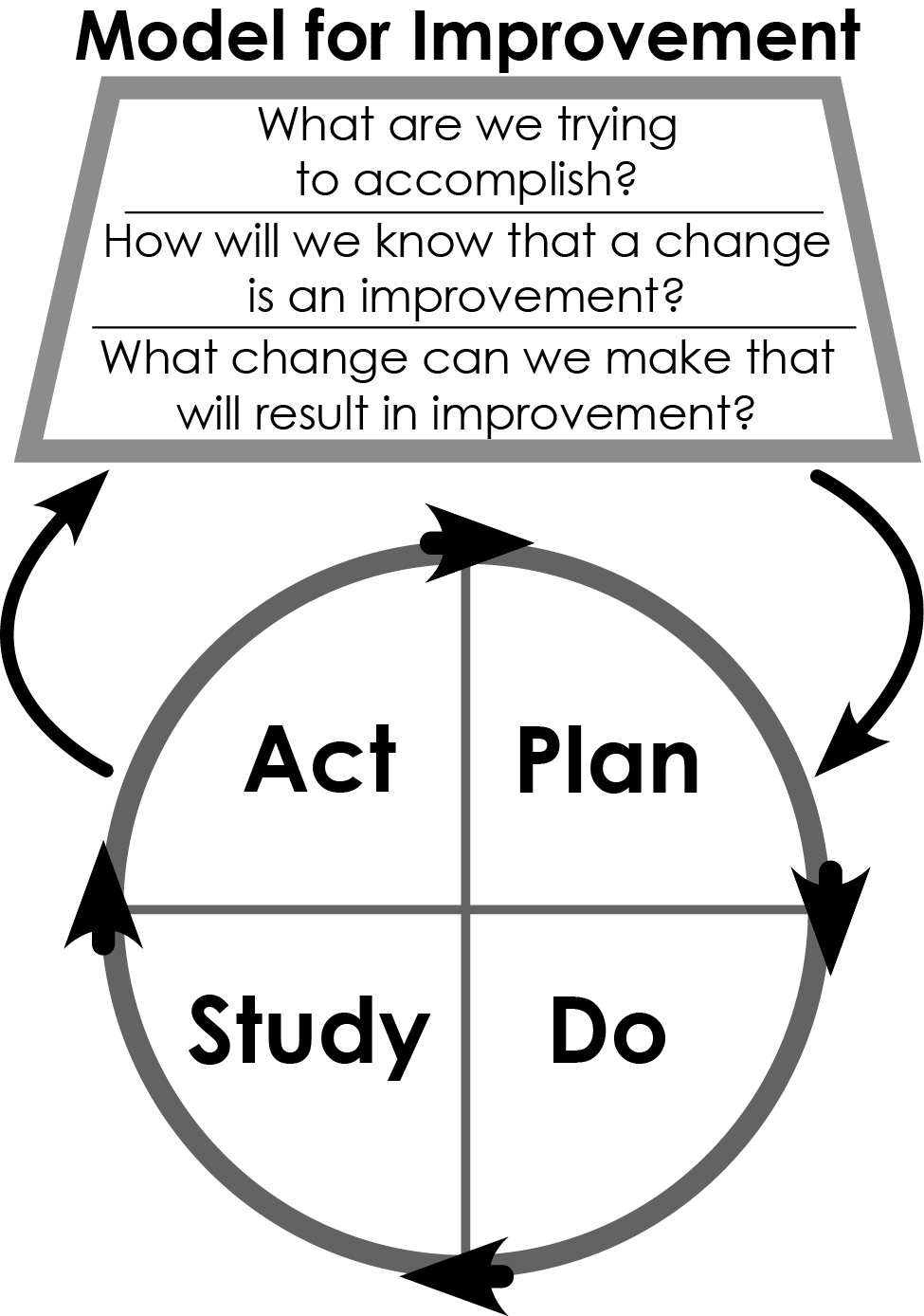
The fundamental approach that serves as the basis for most process improvement models is known as the PDSA cycle, which stands for Plan, Do, Study, Act. As illustrated in Figure 4-1, this cycle is a systematic series of steps for gaining valuable learning and knowledge for the continual improvement of a product or process. Underlying the concept of PDSA is the idea that microsystems and systems are made up of interdependent, interacting elements that are unpredictable and nonlinear in operation. Therefore, small changes can have large effects on the system.
Figure 4-1. Plan-Do-Study-Act Cycle
The cycle has four parts:
- Plan. This step involves identifying a goal or purpose, formulating an intervention or theory for change, defining success metrics and putting a plan into action.
- Do. This is the step in which the components of the plan are implemented.
- Study. This step involves monitoring outcomes to test the validity of the plan for signs of progress and success, or problems and areas for improvement. Short-cycle, small-scale tests, coupled with analysis of test results, are helpful because microsystems or teams can learn from these tests before they implement actions more broadly.7,8
- Act. This step closes the cycle, integrating the learning generated by the entire process, which can be used to adjust the goal, change methods, or even reformulate an intervention or improvement initiative altogether.
The PDSA cycle involves all staff in assessing problems and suggesting and testing potential solutions. This bottom-up approach increases the likelihood that staff will embrace the changes, a key requirement for successful QI.9
When you are ready to apply the PDSA cycle to improve performance on CAHPS scores, you will need to decide on your goals, strategies, and actions, and then move forward in implementing them and monitoring your improvement progress. You may repeat this cycle several times, implementing one or more interventions on a small scale first, and then expanding to broader actions based on lessons from the earlier cycles.
4.B.1. Plan: Develop Goals and Action Plan
This section discusses four key steps in the planning stage of a PDSA cycle as part of a CAHPS-related quality improvement process:
- Establish improvement goals.
- Identify possible strategies.
- Choose specific interventions to implement.
- Prepare a written action plan.
4.B.1.a. Establish Improvement Goals
The team's first task is to establish an aim or goal for the improvement work. By setting this goal, you will be better able to clearly communicate your objectives to all of the sectors in your organization that you might need to support or help implement the intervention.
The goal should reflect the specific aspects of CAHPS-related performance that the team is targeting. It should also be measurable and feasible. One of the limitations of an annual CAHPS survey as a measurement tool is the lag time between the implementation of changes, the impact on people’s experiences, and the assessment of that impact. For that reason, the team needs to define both ultimate goals as well as incremental objectives that can be used to gauge short-term progress. After defining your ultimate goals, ask 'What is the gap between our current state and our goals?' Make of list of those gaps and use them to make SMART (specific, measurable, achievable, realistic, and time bound) incremental objectives.
For example, a team concerned about improving performance on the 'Getting Timely Appointments, Care, and Information' composite measure in the Clinician & Group Survey may set a 1-year goal of a two percent increase in its composite score. At the same time, it could specify goals for the number of days it takes to get an appointment for non-urgent and urgent visits. Similarly, a team focusing on overall ratings may set goals for complaint rates for the health plan as a whole or for individual medical groups and then review those rates monthly.
4.B.1.b. Identify Possible Strategies
With objectives in place, the next task of the team is to identify possible interventions and select one that seems promising. Keep in mind that all improvement requires making a change, but not all changes lead to improvement.
Section 6 of this Guide presents a number of different strategies that health care organizations can use to improve different aspects of their CAHPS performance. In addition, you may want to consult several case studies of health care organizations that have implemented strategies to improve performance on CAHPS scores.
These sources of improvement ideas offer an excellent starting point, but they are by no means comprehensive. There are many other sources for new ideas or different ways of doing things both within and outside of health care. Consequently, improvement teams should make an effort to develop and maintain systematic ways of identifying effective solutions.
New ideas and innovative solutions can be found:
- At conferences or workshops.
- In the academic literature, the media, and/or the popular press.
- Through the identification of benchmark practices in health care as well as other industries, i.e., noncompetitive benchmarks.
- Through patients and their families—whether through direct interviews and focus groups, as partners on quality improvement teams, or as members of Patient and Family Advisory Councils.
- In the Agency for Healthcare Research and Quality's searchable clearinghouse of health care innovations.
One useful way to develop and learn innovative approaches is to visit other health care organizations. Resistant or hesitant staff members are often 'unfrozen' by visiting another highly respected site that has successfully implemented a similar project. You can also visit a company outside of the health care industry to get new ideas. Some health plans, for example, have learned how to improve their call center operations by sending staff to visit mail-order catalog houses or brokerage firms. The Cleveland Clinic has required every doctor and senior administrator to make one 'innovation site visit' a year to learn about different approaches that can be brought home and tested.
—Plsek P. Innovative thinking for the improvement of medical systems. Ann Intern Med 1999;131:438-44. Available at http://annals.org/article.aspx?articleid=712942. Accessed July 27, 2015.
4.B.1.c. Choose Specific Interventions To Implement
To decide which new ideas or benchmark practices to implement, the improvement team needs to consider several factors:
- Compatibility with the organization and local culture. Serving Cuban coffee in the waiting room of the clinics of a Miami medical group may be very patient-friendly, for example, but it is not likely to be viewed with the same enthusiasm by patients in Arizona or Massachusetts.
- Technical merit. The ideas that are most likely to be adopted are those that provide significant advantages over existing practices for both patients and providers—whether in the form of increased efficiency, higher patient and employee satisfaction, or improved outcomes. All improvement efforts ultimately have to answer the question: 'What's in it for me?'
- Fit with the problem. The best intervention will be one that suits the specific problem you need to address (or can be tailored as needed). To ensure a good fit, the improvement team should seek input from both affected staff as well as patients or members. If you ignore either source of information in your planning, you may choose an intervention that will not fix the real problem.
Depending on the nature of the intervention, you may want to break it down into a set of related but discrete changes. For example, if the team decides to implement a new specialist referral process, you could begin by making changes to the procedures used to communicate with the specialist's office. The communication process with the health plan might then be the target of a separate change.
4.B.1.d. Prepare a Written Action Plan
Although there is no one 'correct' way to write an action plan for your organization or facility, it is important to have some form of written document that states your goals, lists your overall strategies to achieve those goals, and then delineates the specific actions you will take to implement the interventions you have selected to address the identified problems. One way to organize the action plan is to review the following key questions as a team and document your answers:
- What areas do you want to focus on for improvement?
- What are your goals?
- What initiative(s) will you implement? Describe the specific actions briefly.
- Who will be affected, and how?
- Who can lead the initiative? Identify a leader and/or champion to manage the project.
- What resources will be needed?
- What are possible barriers, and how can they be overcome?
- How will you measure progress and success? Specify the measures you plan to use to monitor progress in achieving the desired changes to organizational processes and CAHPS scores. Read more about measures below.
- What is the timeline? Record your planned start and end dates for the action.
- How will you share your action plan?
It also helps to lay out the calendar for all actions in a Gantt chart format, so you can verify that the timing of sets of actions makes sense and is feasible to complete with the staff you have available.
4.B.2. Do: Select Measures To Monitor Progress
When a team establishes its goal, it typically specifies one or more performance metrics to assess whether a change actually leads to improvement. These measures should be clearly linked both to the larger goal and to the intervention itself. For example, if the goal is to speed specialist referrals, you could measure the time it takes to get a response from the specialist's office or an approval from the health plan.
Resources on Measurement- Institute for Healthcare Improvement. Science of Improvement: Establishing Measures. Available at http://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovementEstablishingMeasures.aspx
- Carey RG, Lloyd RC. Measuring Quality Improvement in Healthcare: A Guide to Statistical Process Control Applications. New York: American Society for Quality; 1995.
- Wheeler D. Understanding Variation: Keys to Managing Chaos. Knoxville, TN: Statistical Process Controls, Inc.; 1993.
- American Board of Internal Medicine (ABIM) Foundation. Putting Quality Into Practice video series. This series shows the perspectives of physicians who have adopted quality measurement and improvement tools. The doctors speak candidly about why they decided to measure their performance, and how the information empowered them to improve the care they provide to patients.
4.B.2.a. Tips on Selecting Measures
Choose measures that allow you to track each of three steps in the improvement process:
- Test the acceptance and/or adherence to new or revised practices.
- Examine how and how much the new practices are affecting the delivery of patient-centered care.
- Assess how much patient experience of care is improving.
Communicate with staff about why the measures are being collected and how these data will help improve their quality of work life and the patient’s experience.
Seek a feasible number of measures that address the most important aspects of the improvements you are trying to achieve. Too many measures could create a burden on the staff, leading to loss of attention due to information overload; too few measures may omit tracking of important aspects of the changes you are making.
4.B.2.b. Producing Visual Displays
Once you have established practical measures, you will be able to produce visual displays of your performance over time by tracking the metric on control or run charts. Control and run charts are helpful tools for regularly assessing the impact of process improvement and redesign efforts: monthly, weekly, or even daily. In contrast to tables of aggregated data (or summary statistics), which present an overall picture of performance at a given point in time, run and control charts offer an ongoing record of the impact of process changes over time.
A run chart can show different data collection points plotted over time for a specific survey question, e.g., an item about patients' ability to reach the practice by phone. By measuring and tracking results to this question at regular and frequent time intervals, managers can discern how process improvement interventions relate to changes in survey results. If an intervention appears to have positive results, it can be continued and sustained; if not, it can be modified or discontinued.
Dashboard reports are another way to display performance. A dashboard report presents important data in summary form in order to make it easier to identify gap in performance and trend performance against goals. Dashboards can be a useful method for sharing consistent information across multiple levels of an organization. For example, the Massachusetts General Physicians Organization (MGPO) prepares quarterly leadership dashboards with benchmarks and targets, where relevant, at a summary level across clinical services, at the clinical service level, and at the practice level.10
4.B.3. Do and Study: Test and Refine Actions on a Small Scale
Once you have selected interventions, the next stage of the cycle is to develop and test specific changes. It helps to think of this stage as a number of 'mini-cycles' within the larger improvement cycle, in the sense that the microsystem or team is likely to go through multiple iterations of testing and refining before the specific changes add up to a real intervention.
Small-scale tests of the interventions you wish to implement help refine improvements by incorporating small modifications over time. Conducting these small tests of change within a microsystem can be very powerful:
- They allow for incremental modifications of interventions to fix problems, which helps the larger implementation run smoothly.
- Failures are low-risk because you have not tried to change the entire culture.
- You create enthusiasm and positive 'word-of-mouth' for early successes.
- It is easier to accumulate evidence for implementation when people are engaged in making something work rather than focused on the 'failure analysis.'
Most improvement strategies require some adaptation to the culture of the organization. Patient-centered improvement strategies have to consider the needs of patients and their families as well as the staff. Moreover, front-line staff will frequently resist new ideas if they are not allowed to modify them and test their own ideas.
4.B.4. Act: Expand Implementation to Reach Sustainable Improvement
Building off of the development and testing of specific changes, the final stage of the PDSA cycle involve adopting the intervention and evaluating it against the goals of the improvement project and the measures established for tracking improvement progress. For example:
- Did the intervention succeed in reducing the time required to see a specialist?
- Are members and patients reporting better experiences with regards to getting care quickly?

This part of the improvement cycle is really the ongoing work of health care and where your teams will spend most of their time. There are no set rules about how long this part of the cycle takes. It depends in part on how frequently you monitor your CAHPS scores and other quality measures.

It is important not to let the work go on too long without ongoing measurement in order to make sure you are making progress toward achieving your aims. Most monitoring takes place on a monthly or quarterly basis. The team can use data on the impact of the intervention to see if it is making progress towards the goals and to determine whether to conduct a new set of analyses of its CAHPS performance. The purpose of this effort is to get some sense of what worked, what did not work, and what further or new interventions may be needed. To the extent that the improvement initiative was successful, the team must also think about ways to sustain and spread the improvements over time.
Resources on Sustaining and Spreading Improvements- Massoud MR, Nielsen GA, Nolan K, Schall MW, Sevin C. A Framework for Spread: From Local Improvements to System-Wide Change. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2006. (Available at http://www.ihi.org/resources/Pages/IHIWhitePapers/AFrameworkforSpreadWhitePaper.aspx)
- Nolan KM, Schall MA. A framework for spread. In Nolan KM, Schall MW, editors: Spreading Improvement Across Your Health Care Organization. Oak Brook, IL: Joint Commission Resources, 2007,1–24.
- Øvretveit J. Implementing, sustaining, and spreading quality improvement. In The Joint Commission: From Front Office to Front Line: Essential Issues for Health Care Leaders, 2nd ed. Oak Brook, IL: Joint Commission Resources, 2012, 159–176.
4.B.4.a. Identify and Deal With Barriers
Healthcare Quality Improvement Tools
As part of its work, the team will need to take a hard look at the psychological, physical, and procedural barriers it has to address in order to accomplish its aim. Barriers to improvement come in many guises. Psychological barriers such as fear of change, fear of failure, grief over loss of familiar processes, or fear of loss of control or power can be significant impediments to overcome. Other common barriers include the following:
- Lack of basic management expertise.
- Lack of training in customer service, quality improvement methods, or clinical areas such as doctor-patient communication.
- Inadequate staffing levels.
- Poor information technology systems.
- Outdated or misguided organizational policies. For example, many organizations are so concerned about violating HIPAA regulations that they do not want to give information to a patient about their own care for fear of violating patient confidentiality.
Despite the serious nature of some of these barriers, few are large enough to bring a project to a halt. Typically, they are cited as excuses for two of the fundamental barriers to change: the fear of new ways of doing things and the fear of failure.
Anticipating How the Improvement Process Affects StaffAn improvement process often requires significant changes in people’s attitudes and behaviors, often requiring staff to give up their old standards and practices and adopt new ones. As a result, you can expect pushback from some staff as you introduce new processes and habits.
Many staff will 'get it' early and pitch in enthusiastically. But introducing and reinforcing changes in behavior that 'stick' in the form of sustainable practices will take some work and time to succeed. Over time, as less enthusiastic staff see positive progress, they too will become more engaged and supportive.
When you succeed, the payoff is significant, with benefits not only for patients but also for clinicians and staff. Many organizations have found that job satisfaction for their staff rises with improved patient experiences because the new, better practices usually reduce frustrating inefficiencies in the system that created extra work for staff.
Learn More: Aligning Forces for Quality. The Center for Health Care Quality at the George Washington University Medical Center School of Public Health and Health Services. Good for Health, Good for Business: The Case for Measuring Patient Experience of Care. 2012.Available at http://forces4quality.org/case-patient-experience.
4.B.4.b. Identify and Cultivate Facilitators
The team also needs to identify factors that could facilitate their work. Facilitators can include financial or nonfinancial incentives, such as gain sharing for staff if a specific target is met or better quality of life for the staff when a problem is fixed. Other facilitators include picking an aim that is part of the organization's strategic plan or one that will improve other goals the staff care about, such as clinical outcomes.
Sometimes, the facilitator is the ability of a change to help achieve secondary goals. For example, improvements in doctor-patient communication may decrease medication errors, or the development of shared care plans may improve clinical outcomes and reduce no-shows for appointments or procedures.
Pdsa Description
4.B.4.c. Harness Social Interaction to Spur Adoption of Innovations
Research on the diffusion of innovation has found that social interaction plays a crucial role. Most people do not evaluate the merits of an innovation on the basis of scientific studies; they depend on the subjective evaluations of 'early adopters' and model their behaviors after people they respect and trust.11 For that reason, choosing the right team members and opinion leaders (i.e., people within an organization who informally influence the actions and beliefs of others) is critical to efforts to diffuse innovation.
Depending on the project, you may want to try to identify the opinion leaders that would be helpful to involve (assuming they are open to change and new ideas). Interpersonal communication works best when the people communicating the message are respected opinion leaders within the same staff group whose behavior they are trying to change. For example, an innovation to change the behavior of receptionists will often move quickly if it is led by a respected receptionist or office manager. But this person would probably not be as effective at getting physicians in a medical group to change their communication style with patients.
Ask people whose opinion they respect. Who do they follow when they have adopted new clinical or improvement practices? Who do your staff look to when they want advice or information about the organization?
4.B.4.d. Communicate Internally
One important step that is often neglected is the communication of successes throughout the organization—to organizational leaders as well as clinical and administrative staff. By discussing successful projects, the team helps to reinforce the culture of quality improvement, build credibility for the intervention, reward those involved, and foster the spread of effective innovations.
The organization's leaders can also:
- Use media and interpersonal communication to promote the work of specific improvement teams.
- Highlight successful innovations in staff newsletters and in staff and board meetings.
- Reinforce the importance of the project by sitting in on improvement team meetings or visiting the practice site or unit involved in the project.
A related practice is the communication of changes beyond the walls of the organization to members or patients. By telling people about innovative practices—whether through newsletters, emails, office computer screensavers, member Web sites, or handouts in the office—you can raise the standard of expectations.
Learn About Encouraging Innovation- Blakeney B, Carleton P, McCarthy C, Coakley E. Unlocking the Power of Innovation. OJIN: The Online Journal of Issues in Nursing. 2009 May 31;14(No. 2, Manuscript 1). Accessible at http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol142009/No2May09/Innovation.html. This article describes innovative methods and highlights specific examples of organizational structures that support innovations within health care organizations.
- Christensen C, Bohmer R, Kenagy J. Will disruptive innovations cure health care? Harv Bus Rev 2000 Sep-Oct;78(5):102- 12, 1999.
- Langley GJ, Nolan KM, Norman C, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco: Jossey-Bass; 1996.
- Kelley T, Littman J. The 10 Faces of Innovation: IDEO’s Strategies for Beating the Devil’s Advocate & Driving Creativity Throughout Your Organization. New York: Doubleday; 2005.
- Plsek PE. Innovative thinking for the improvement of medical systems.Ann Intern Med 1999;131(6): 438-44.
- Plsek PE. Thinking differently. Available at: National Health Services Institute for Innovation and Improvement. http://www.institute.nhs.uk/building_capability/new_model_for_transforming_the_nhs/thinking_differently_guide.html. Accessed May 28, 2015.
- Rogers E. Diffusion of innovations. 5th ed. New York City: Free Press, 2003.
Pdsa Cycle Powerpoint Presentations
Return to Contents
Proceed to Next Page of Section 4
Page originally created November 2015